- Pediatric Hematology-Oncology
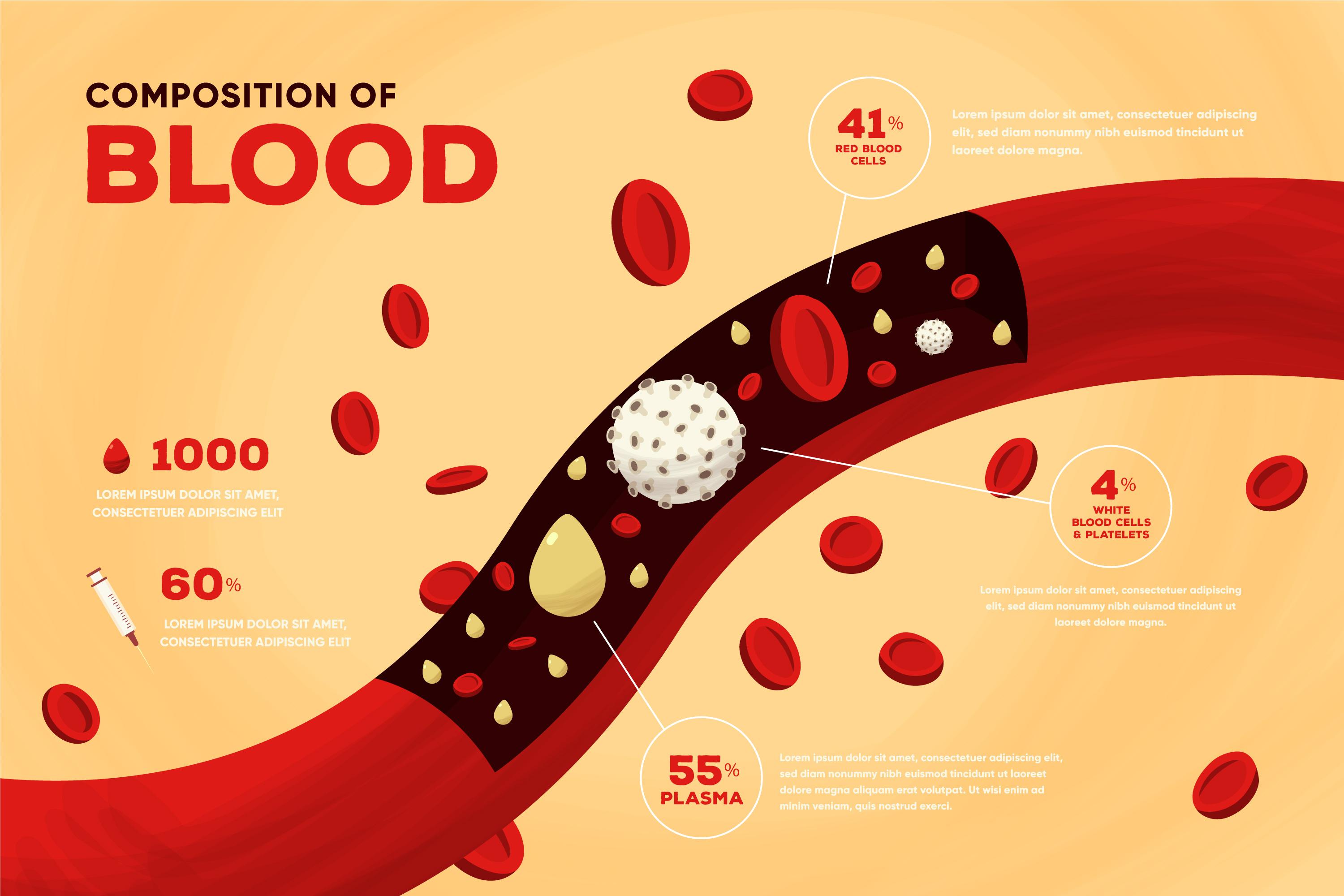
Pediatric hematology-oncology, led by pediatric hematologist-oncologists, focuses on diagnosing and treating blood disorders and cancers in children. Conditions such as leukemia, lymphoma, thalassemia, and bone marrow failure syndromes are managed through advanced treatments like chemotherapy and bone marrow transplantation (BMT). Early detection through specialized diagnostic techniques and timely intervention are critical for improving outcomes in pediatric patients.
Expertise in Pediatric Hematology-Oncology
What is Pediatric Bone Marrow Transplantation?
“Bone marrow transplantation (BMT) is a life-saving procedure used to treat children with severe blood disorders and cancers, such as leukemia, lymphoma, and thalassemia. It involves replacing damaged or diseased bone marrow with healthy stem cells, either from the patient (autologous) or a donor (allogeneic). The procedure requires meticulous planning, including stem cell harvest, conditioning regimens, and post-transplant care to manage complications like graft-versus-host disease (GVHD) and infections.”
How Does Bone Marrow Transplantation Work?
BMT works by infusing healthy stem cells into the patient’s bloodstream, which then migrate to the bone marrow to produce healthy blood cells. Under the care of a pediatric hematologist-oncologist, the process involves pre-transplant conditioning with chemotherapy to eliminate diseased cells, followed by stem cell infusion. Post-transplant, patients are closely monitored for complications like infections, graft failure, or GVHD. Advances in matched unrelated donor (MUD) and haploidentical transplants have improved outcomes for pediatric patients.


Key treatment modalities in pediatric hematology-oncology include:
- Chemotherapy and Targeted Therapies
- Bone Marrow and Stem Cell Transplantation
- Immunotherapy and Molecular Diagnostics